The placenta from full-term pregnancies and extraembryonic tissues such as fetal membranes and the umbilical cord represent an ethically accessible and easily obtainable source of stem cells. These tissues provide various populations of stem cells, known as perinatal cells, including mesenchymal stem cells (MSCs) and other cell types with stemness potential, such as epithelial cells derived from the amniotic membrane (AECs). AECs exhibit remarkable plasticity, with the ability to differentiate into tissues originating from all three germ layers, including cardiac, neural, and pancreatic tissues. The isolation and characterization of these cells open promising perspectives for applications in tissue engineering and cell therapy for degenerative diseases. Moreover, there is growing interest in developing innovative approaches to cell cultures that better mimic in vivo conditions. Three-dimensional (3D) cultures, such as spheroids and organoids, offer significant advantages over traditional two-dimensional (2D) cultures. These 3D systems recreate a more physiologically relevant tissue microenvironment by incorporating extracellular matrix components and promoting cell to cell interactions, ultimately enhancing the study of stem cell characteristics and their therapeutic applications.
At our center, the study of perinatal stem cells is divided into three different branches, illustrated below. These areas benefit from the close collaboration and support of patient associations, specifically Associazioni Giovani Diabetici – AGD Bologna (https://agdbologna.com/) for type 1 diabetes and Conquistando Escalones Association – ACE (http://www.conquistandoescalones.org/) for muscular dystrophies.
Study of the Differentiation Potential and Immunomodulatory Capacity of Perinatal Stem Cells for the Treatment of Type 1 Diabetes
Type 1 diabetes mellitus (T1DM) is an autoimmune disease in which the immune system destroys pancreatic beta cells, leading to chronic insulin deficiency. Although insulin therapy effectively controls symptoms, it does not address the cause, which is linked to persistent inflammation and immune dysfunction.
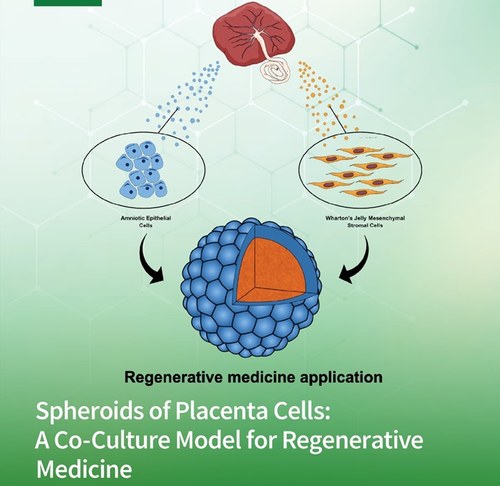
Perinatal stem cells, such as human amniotic epithelial cells (hAECs) and mesenchymal stromal cells from Wharton's jelly (hWJ-MSCs), show therapeutic potential due to their immunomodulatory, anti-inflammatory, and regenerative properties. In three-dimensional (3D) cultures, these cells can enhance cellular interactions, potentially promoting insulin release and protecting pancreatic beta cells from autoimmune attacks.
This project aims to develop an innovative preclinical model using 3D spheroids composed of hAECs and hWJ-MSCs. The goal is to simultaneously address the immunological causes of T1DM while integrating tissue regeneration and immune system modulation.
Study of the Immunomodulatory Effect of Perinatal Stem Cells in Muscular Dystrophies
Inflammation plays a key role in regenerative processes, but in many muscular dystrophies (MDs) the degeneration of myofibers leads to the constant release of their contents, triggering chronic inflammation that contributes to disease progression. Additionally, studies on MDs highlight significant variability in immune responses, suggesting that endogenous immunomodulators may regulate immune activity differently depending on the specific type of MD.
In this context, the transplantation of mesenchymal stem cells (MSCs), such as those isolated from the umbilical cord and derived from Wharton's jelly, represents a promising therapeutic strategy for various rare diseases. These cells promote tissue regeneration and repair through paracrine signaling, mediating anti-inflammatory, antifibrotic, and pro-regenerative effects.
The aim of this study is to analyze the immunomodulatory properties of perinatal MSCs and develop three-dimensional culture models that include both healthy myoblast progenitors and those derived from degenerative muscular diseases, with the goal of optimizing therapeutic strategies for these conditions.
Biophysical Characterization of Perinatal Cells
In this study, we investigate the potential of emerging microfluidic technologies to gain new insights into the biophysical characteristics (e.g., density, shape, and size) of stem cells isolated from perinatal sources, starting from heterogeneous samples or 3D cultures. The prospective application of these technologies to the study of perinatal cell populations could contribute to the development of new biopharmaceutical strategies based on innovative and safe cell therapy approaches.
Microfluidic analysis enables the investigation of cellular phenotypes while maintaining physiological conditions. This expanding field has already led to the development of portable diagnostic systems, lab- on-a-chip platforms for drug discovery and screening, tools for basic life sciences research, and sophisticated analytical devices. In the future, microfluidic technologies are expected to bring significant advancements in the production and quality control of cellular products, such as extracellular vesicles, which are considered promising drug delivery systems.
The renewed interest in the biophysical properties of cells in vitro will allow for the refinement of developing microfluidic technologies, focusing on the biomechanical aspects of tissue engineering, the remodeling of the stem cell niche, and extracellular matrix signaling. The goal of this research is to achieve a more precise definition of the cellular microenvironment, including the physical forces that govern cell state and behavior.